Roche's tocilizumab cuts deaths in hospitalised COVID-19 patients - study
By Kate Kelland
LONDON, Feb 11 (Reuters) - Roche's arthritis drugtocilizumab cuts the risk of death among patients hospitalisedwith severe COVID-19, also shortening the time to recovery andreducing the need for mechanical ventilation, results of a largetrial showed on Thursday.
The findings - from the RECOVERY trial, which has beentesting a range of potential treatments for COVID-19 since March2020 - should help clear up confusion about whether tocilizumabhas any benefit for COVID-19 patients after a slew of recentmixed trial results.
"We now know that the benefits of tocilizumab extend to allCOVID patients with low oxygen levels and significantinflammation," said Peter Horby, a professor of emerginginfectious diseases at Oxford University and the joint leadinvestigator on the RECOVERY trial.
In June last year, the RECOVERY trial found that the cheapand widely available steroid dexamethasone reduced death ratesby around a third among the most severely ill COVID-19 patients.That drug has since rapidly became part of standard-of-carerecommended for severe patients.
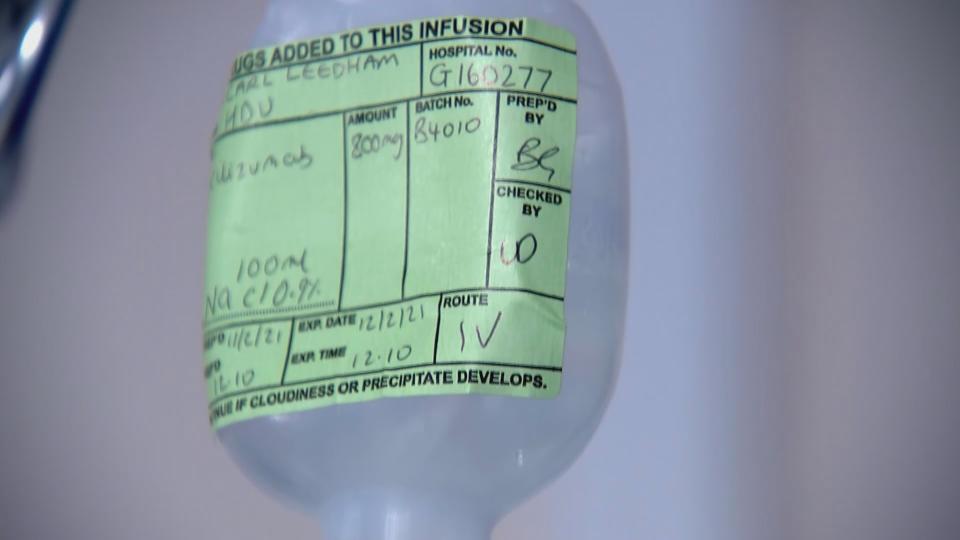
Tocilizumab, sold under the brand name Actemra, is anintravenous anti-inflammatory monoclonal antibody drug used totreat rheumatoid arthritis. It was added to the trial in April2020 for patients with COVID-19 who required oxygen and hadevidence of inflammation.
The study data were from 2,022 COVID-19 patients who wererandomly allocated to receive tocilizumab by intravenousinfusion and who were compared with 2,094 patients randomlyallocated to usual care alone. Researchers said 82% of allpatients were taking a systemic steroid such as dexamethasone.
Results showed that treatment with tocilizumab significantlyreduced deaths - with 596 (29%) of the patients in thetocilizumab group dying within 28 days, compared with 694 (33%)patients in the usual care group.
This translates to an absolute difference of 4% and meansthat for every 25 patients treated with tocilizumab, oneadditional life would be saved, Horby and his co-leadinvestigator Martin Landray said.
They added that benefits of tocilizumab were clearly seen tobe in addition to those of steroids.
"Used in combination, the impact is substantial," saidLandray, who is also an Oxford professor of medicine andepidemiology.
He added that results "clearly show the benefits oftocilizumab and dexamethasone in tackling the worst consequencesof COVID-19 – improving survival, shortening hospital stay, andreducing the need for mechanical ventilators."
Roche's drug division chief Bill Anderson said lastweek that previous mixed results were likely due to differencesin the type of patients studied, when they were treated, and theendpoint - the juncture at which success or failure is measured.
"We think we're sort of zooming in on both the most relevantendpoints and relevant patient population," Anderson said. "Itseems like the ideal candidates are patients who are really inthat acute phase of inflammatory attack."
Actemra, along with Sanofi's similar drug Kevzara,was authorized by Britain's NHS in early January for COVID-19patients in intensive care units after preliminary data from asmaller study called REMAP-CAP indicated it could reducehospital stays by about 10 days.
During 2020, Actemra rose to become Roche'sfifth-best-selling drug, at more than $3 billion, with nearly$600 million from COVID-19 treatment.(Reporting by Kate Kelland in LONDON, with additional reportingby John Miller in ZURICH. Editing by David Evans)
